Entry 5 – Evidence & Epidemiology (October 2021)
Posted in: Journal
Research is formalised curiosity. It is poking and prying with a purpose.”
Zora Neale Hurston, American Anthropologist, author and film maker 1891 – 1960
In this blog I want to talk about what I mean when I say that this Review will be evidence-based, and to explain how evidence is used in clinical practice.
To take a familiar example, through the Covid pandemic everyone has learnt a lot more about how science is used to guide everything from diagnosis through to treatment. Anyone who listened to the daily Covid briefings rapidly learnt that medicine is a business which is full of uncertainties and new learning. The public learnt that continuous cough, fever and loss of smell were common presentations of Covid-19, but then we learnt that sometimes people with Covid could be asymptomatic. Lateral flow tests were good for screening, but could give false negatives (you had a negative test but still had Covid) or more rarely false positives (you had a positive test but didn’t have Covid), whilst the PCR test remained the more accurate ‘gold standard’. Treatment of seriously ill Covid patients improved as patients were kept for longer on less intensive forms of breathing support, and different medicines were trialled. And meanwhile everyone waited anxiously for the results of the vaccine trials.
In the background, another group of clinicians and scientists started to appear on our TV screens – not the front-line clinicians, or the specialist virologists, but the epidemiologists; the specialists who look at patterns of health, disease and wellbeing in the population. Importantly in relation to Covid, they started to tell us who was most vulnerable, whether because of their age, their ethnic background, or underlying illnesses. That meant that when the vaccines were ready to be used, it was not a case of one size fits all – those at greatest risk would be vaccinated first. At the other end of the scale, it was not clear whether children would benefit from vaccination at all, and some of the most interesting lessons have been over the last few weeks as the decision has been made about vaccinating 12-15 year olds. The JCVI (Joint Committee on Vaccination and Immunisation) looked purely at the medical benefits and harms; they found that the medical benefits only marginally outweighed the harms. But when the Chief Medical Officers looked at wider issues like missing school and mental health impacts, the balance tipped in favour of vaccination.
So, what relevance does all this have in talking about the evidence base for treating young people with gender-related distress? In this blog I want to explore two issues:
The first issue that I want to tackle is the often heated discussion about whether or not hormone treatment for young people with gender dysphoria is experimental. If we return to the learning from Covid as an example, Dexamethasone was not experimental when used for other conditions for which it was already known to be effective, but was experimental when used for Covid, until the data proved it to be safe and effective.
None of the hormone treatments currently being given to children and young people with gender dysphoria are being administered as part of a formal clinical trial. This means that the question we have to ask is about the strength of the existing evidence on the benefits versus the harms. We do have some data on the shorter-term physical and mental health outcomes of these treatments, but of course we could not reasonably expect this to have the precision of the data on Covid vaccination of 12-15 year olds which was based on very large clinical trials. However, the biggest gap in the evidence is in terms of longer-term outcomes into adulthood. It was for this reason that the recent NICE review of the evidence did not lead to a definitive policy recommendation. So, I’m really pleased to be able to let you know that we have appointed a team from the University of York to conduct the academic research that will help us fill some of these data gaps. In future communications I will be discussing in more detail what the current evidence base tells us, the limitations of the data, and what we can do to strengthen that evidence so that clinicians, young people and their families have the best possible information.
Secondly, I want to talk about epidemiology. We have very clear information from the GIDS service in the UK, and from other international services, that the mix of young people presenting to services for gender-questioning young people has changed substantially and rapidly in the last 5-10 years:
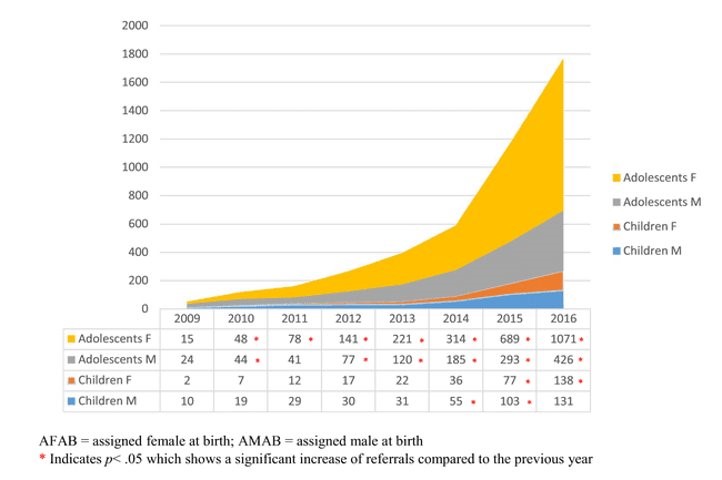
Figure 1 – Sex ratio in children and adolescents referred to GIDS in the UK(2009 – 2016). (De Graaf NM, Giovanardi G, Zitz C, Carmichael P. Arch Sex Behav. 2018;47(5):1301-1304.)
Data on current referral rates can be found here: https://gids.nhs.uk/number-referrals.
Previously the GIDS service saw approximately 50 young people per annum, who were predominantly birth registered boys who had experienced gender incongruence from a very early age. From about 2014 onwards the numbers increased exponentially and now exceed 3000 per annum, predominantly birth registered girls in early teens who have expressed their gender incongruence much later. At this stage we don’t fully understand why this change has occurred, although there are many different and conflicting views about how to explain it. And of course, we have even less longer-term information about this group’s journey into adulthood.
Alongside these changes, many more young people are identifying as non-binary or gender fluid and may have quite distinct needs from those who express a strong trans binary preference. Once again, we have limited data on the short-term needs or long-term outcomes for this group.
Taking time to understand the epidemiology will be important, because as with any other situation where there is clinical intervention, it means there will not be a ‘one-size-fits-all’ approach to assessment, support and intervention. Each young person will need an individualised approach to find the right pathway for them. I believe that our evidence-based approach will add significantly to the international evidence in this area and importantly for the review, it will help inform recommendations on how to improve clinical support and provide appropriate treatment for the children and young people who need timely access to NHS services.
